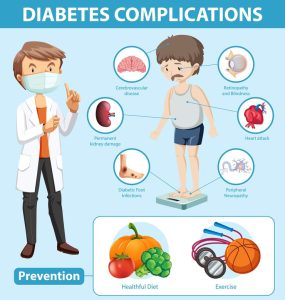
Uncontrolled type 2 diabetes can have severe consequences on the cardiovascular system. High blood sugar levels damage blood vessels and nerves, accelerating atherosclerosis and increasing the risk of heart attacks, strokes, and peripheral artery disease.
Type 2 diabetes, characterized by insulin resistance and impaired glucose regulation, doesn’t confine its impact solely to blood sugar management. It poses a dual challenge to health by significantly increasing the risk of cardiovascular complications. The intricate interplay between diabetes and the cardiovascular system sets the stage for a range of disorders, emphasizing the importance of comprehensive management to mitigate these risks.
Chronically elevated blood sugar levels in individuals with type 2 diabetes contribute to the development of atherosclerosis—the narrowing of arteries due to the accumulation of plaques. This process is accelerated by the presence of additional risk factors such as hypertension and dyslipidemia, common companions to diabetes. Atherosclerosis not only affects the coronary arteries, leading to coronary artery disease and an increased risk of heart attacks, but also extends its reach to other vital vessels, potentially causing strokes and peripheral artery disease.
The endothelium, the inner lining of blood vessels, plays a pivotal role in vascular health. In diabetes, persistent hyperglycemia impairs endothelial function, reducing the ability of blood vessels to dilate and regulate blood flow. This endothelial dysfunction contributes to the initiation and progression of atherosclerosis, further compromising cardiovascular health.
Type 2 diabetes is intricately linked to hypertension, forming a dangerous synergy that intensifies the strain on the cardiovascular system. Elevated blood pressure, common in individuals with diabetes, places additional stress on the arterial walls, exacerbating the development of atherosclerosis and increasing the risk of heart failure.
Moreover, diabetes significantly raises the risk of developing heart failure, a condition where the heart struggles to pump blood effectively. The structural and functional changes in the heart muscle, often referred to as diabetic cardiomyopathy, are independent of other cardiovascular risk factors. Chronic exposure to high glucose levels contributes to the accumulation of advanced glycation end products (AGEs), which alter the structure and function of proteins, including those in the heart.
Type 2 diabetes also heightens the likelihood of thrombotic events. Diabetes-induced changes in blood composition make it more prone to clot formation. These clots can obstruct blood vessels, leading to heart attacks or strokes. The prothrombotic state associated with diabetes underscores the importance of antithrombotic strategies in managing cardiovascular risk in individuals with diabetes.
Management of type 2 diabetes and its associated cardiovascular risks necessitates a comprehensive approach. Tight glycemic control, achieved through lifestyle modifications, medications, and insulin therapy when needed, is fundamental. Lifestyle interventions, including a heart-healthy diet, regular physical activity, and weight management, play a crucial role in mitigating cardiovascular risks.
![]()
Regular monitoring of blood pressure and cholesterol levels is essential, and medications may be prescribed to manage these parameters effectively. Aspirin therapy, under the guidance of healthcare professionals, may be recommended for its antiplatelet effects, reducing the risk of clot formation.
In conclusion, the relationship between type 2 diabetes and cardiovascular complications underscores the need for integrated care. Addressing both the metabolic and cardiovascular aspects of diabetes is crucial for preserving overall health and preventing life-threatening complications. A holistic approach that combines glycemic control, lifestyle modifications, and cardiovascular risk management is essential in navigating the dual challenge posed by type 2 diabetes to the cardiovascular system.


